Introduction to Dopamine
- Introduction to Neurotransmitters
- The Role of Dopamine
- The Role of Serotonin
- Interplay of Dopamine and Serotonin
- Competing Actions
- Collaborative Actions
- Conflicting Actions on Same Behaviors
- Complexity in Neuronal Combinations
- The Impacts of Therapeutic Drugs on Dopamine and Serotonin
- Dopamine, Serotonin and Mental Health
- Dopamine, Serotonin and Cognitive Functioning
- Settings, Synaptic Plasticity and Sensitization
- Prospects and Challenges in Dopamine & Serotonin Research
Conflicting Actions on Same Behaviors
Obsessive-Compulsive Disorder: The Role of Dopamine and Serotonin
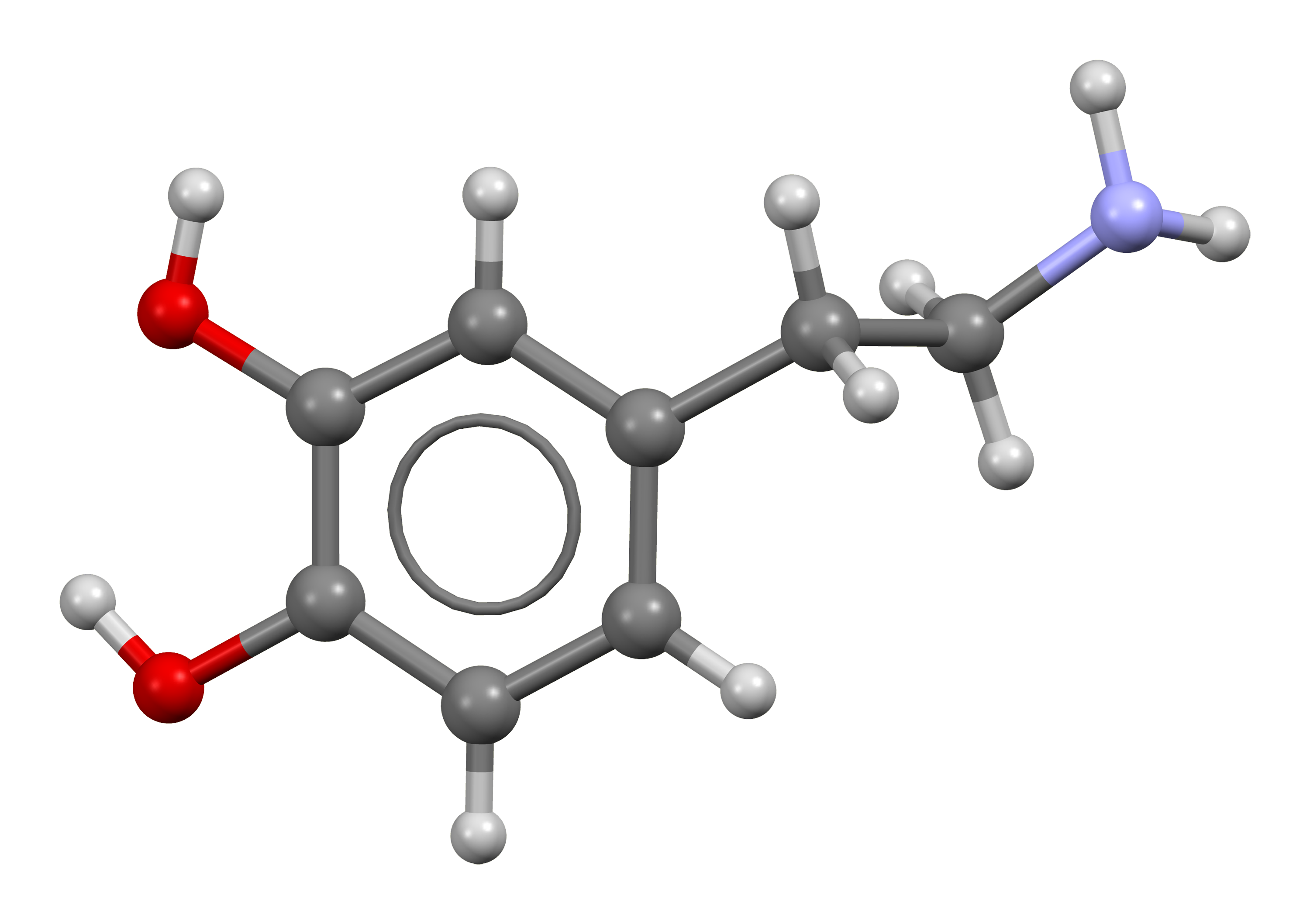
Organic chemical that functions both as a hormone and a neurotransmitter.
Obsessive-Compulsive Disorder (OCD) is a chronic and long-lasting disorder in which a person has uncontrollable, reoccurring thoughts (obsessions) and behaviors (compulsions) that he or she feels the urge to repeat over and over. OCD is typically diagnosed when these obsessions and compulsions become so severe that they interfere with daily life.
Symptoms and Diagnosis of OCD
The symptoms of OCD can vary widely from person to person, but they generally fall into two categories: obsessions and compulsions. Obsessions are unwanted and intrusive thoughts, images, or urges that cause distress or anxiety. Compulsions are behaviors that a person feels compelled to perform in order to ease their distress or anxiety, or to prevent a feared event from occurring.
Diagnosis of OCD is typically made through clinical interviews and symptom rating scales. The Yale-Brown Obsessive Compulsive Scale (Y-BOCS) is one of the most commonly used tools for assessing the severity of OCD symptoms.
Role of Dopamine and Serotonin in OCD
Research has suggested that both dopamine and serotonin play significant roles in OCD. Dopamine is often associated with the reward system of the brain and is thought to play a role in the compulsive aspect of the disorder. Some studies have suggested that increased dopamine activity may contribute to the intense urges to perform compulsive behaviors.
Serotonin, on the other hand, is thought to play a role in the obsessive aspect of the disorder. Lower levels of serotonin have been associated with increased anxiety and obsessive thoughts. Some research has suggested that there may be a dysfunction in the serotonin system in individuals with OCD, although the exact nature of this dysfunction is still not fully understood.
Current Treatments for OCD and Their Effects on Dopamine and Serotonin
The most common treatments for OCD are cognitive-behavioral therapy (CBT) and medication. CBT, particularly a type called Exposure and Response Prevention (ERP), has been found to be very effective in reducing OCD symptoms.
Medications used to treat OCD are primarily selective serotonin reuptake inhibitors (SSRIs), which work by increasing the levels of serotonin in the brain. These include drugs like fluoxetine (Prozac), fluvoxamine (Luvox), and sertraline (Zoloft). Some atypical antipsychotics, which affect dopamine levels, are also sometimes used in treatment, particularly for individuals who do not respond to SSRIs.
Research Findings on the Dopamine-Serotonin Conflict in OCD
While both dopamine and serotonin are implicated in OCD, their exact roles and how they interact are still areas of active research. Some studies have suggested that there may be a delicate balance between the two neurotransmitters in the brain, and that disruptions in this balance could contribute to OCD symptoms. However, more research is needed to fully understand this complex interplay and how it can be targeted in treatment.
In conclusion, while we have made significant strides in understanding the neurobiology of OCD, there is still much to learn. As we continue to unravel the complex roles of dopamine and serotonin in this disorder, we can hope to develop more effective treatments to help those suffering from this debilitating condition.